

Contents
Birth Currents contains the latest childbirth, pregnancy, nutrition, postpartum, baby care, and midwifery-related events in Southern California.
she broke the pattern in her family of birth by cesearean
and created the possibility for her daughter to birth normally".
I am a professional labor companion, childbirth educator and aspiring midwife who has been supporting women through childbirth at homebirths, and in hospitals and birth centers for seven years, and have worked as as a Midwife's Assistant/Apprentice at homebirths for two years, and have attended forty births. When I received a call from a man inquiring about childbirth preparation classes and labor support, I was suspicious. Usually, it is the pregnant woman who calls. I was soon to discover that Stan was earnestly seeking support and education to help his wife through labor and birth. Although he said he picked my name out of a directory of 100 other childbirth educators because I lived close to them, I believe it was a divine intervention that brought Stan and Carol to me. We made an appointment for them to interview me as their labor companion. I drove 15 minutes to their home, entered their gated community nestled in the foothills of a beautiful mountain range. Stan, courteous and kind, met me at my car when I entered their driveway. Stan is a soft-spoken, gentle man in his mid-forties with a quiet strength that is very reassuring. Carol is bold and strong, forthright and bawdy. A woman after my own heart. I loved them both immediately. This was Stan's first child, and Carol's third. She had a girl age 8 and a boy, age 6, both born by cesearean section. Stan wanted childbirth classes to prepare himself this being his first birth, and Carol wanted him to be well-prepared and confident since she was determined to "stay at home as long as possible." She told me, "I know I can do this if no one messes with me." She wanted to give birth vaginally and without drugs this time; she was committed to doing it without an epidural (she had made it almost to pushing without pain medication with both of her previous births, and I had complete faith in her ability to do so). They hired me on the spot. We all knew it felt right. I returned to their home three times to teach them labor-coping strategies, to lead Carol guided through birth visualization processes, to inform them of when to go to the hospital and how to time contractions, and to facilitate communication between them; deepening their trust and reliance upon one another. Carol wanted to make sure that Stan was going to be able to handle it when labor got intense and when she, in the passion of labor, would tell him to leave her alone and go away. Stan just quietly smiled and said, "I am not going anywhere." Carol said the classes gave her the confidence she needed to believe that birth could be done the way nature intended.
I felt I needed to prepare Carol for the possibility that this birth also might end in cesearean section; I wanted her to be able to accept whatever happened without feeling like she failed. Carol did not allow herself to feel victimed by her last birth experiences, yet her dissapointment was evident as she as she shared the stories of her cesearean births.
Her first birth started out in a freestanding birth center. She progressed to 8 centimeters after 30 hours of labor (with ruptured membranes) and then stayed there for seven hours. The OB/GYN finally decided to transport her to the hospital where they took her baby daughter by cesearean section. She told me that she could see how fear, lack of trust and support had stopped her contractions cold. Her second pregnancy was also frought with fear. She was bleeding from the 6th month off and on, and had been in the hospital several times during the pregnancy. She and her husband were under a lot of stress because of this. She said her husband "really wanted to have a son", and Carol felt burdened by the pressure of his expectations, while not feeling emotionally supported during her frequent hospitalizations. Carol had returned to the same OB/GYN who had delivered her first baby, hoping this time for a vaginal birth in the watertub at the birth center. By the time she was admitted to the hospital for bleeding for the fourth time that pregnancy, it had become a routine. Her husband and doctor went home to sleep, trusting the nurses would keep an eye on her and figuring she would go home in the morning once her bleeding subsided, as she had the other times. Carol lay in the hospital bed alone, strapped up to an electronic fetal monitor and noticed that she was having contractions. They kept coming. They were not going away. In fact, they were getting stronger with each passing hour of the night. Finally she admitted to herself that she was in real labor--not preterm labor--but she did not call the nurses, as she figured "if they were concerned, they would let me know". Although it wasn't a conscious decison, she was ready to have her baby; she knew he could survive outside her womb and she wanted to end the anxiety of waiting and worrying he would come too soon. She managed to cope for ten hours all alone, laying in the hospital bed on her back, dealing with with the intense back-to-back contractions without any pain medication. Finally, the nurses became concerned with the baby's abnormal heartrate patterns and her continuing contractions. Her doctor was alerted. He checked her, and found she was 8 centimeters! Concerned about the abnormal fetal heartrate pattern, he said the baby couldn't wait any longer to be born. He quickly performed a second cesearean section because of preterm labor and fetal distress. Having a second cesearean was discouraging to Carol. Worse, she felt no one really understood. Not her husband, nor her sisters and mother could understand why she was unhappy--after all, she had a beautiful, healthy baby boy. Each of her sisters had given birth by cesearean two times each. Their mother had given birth by cesearean four times, with every child. Carol told me that this family history, coupled with having a father who was a doctor --who she never questioned-- contributed to her lack of trust in normal birth and her abdication of responsibility for manifesting the birth her heart desired.
Eventually, Carol's first marraige dissolved, and soon after marrying Stan, she became pregnant with baby number three. Her son and daughter were so excited about having a sibling, and Carol was due on her daughter's birthday. Her daughter declared that her little brother would be born her birthday! Carol was determined to have the birth she always wanted, even if it meant staying out of the hospital as long as possible. This time, she was determined to rely upon herself and get the support she needed to do the birth her way.
The birth team for number three was to be Stan, Carol's best friend Cathy who had been at her other two births, and me. The children would be present if it wasn't their weekend with their dad. I accompanied the family to Carol's prenatal visit with her doctor. She was very dissapointed that her former OB/GYN had closed down his birth center and retired, but she told me she really liked her new doctor. A doctor of osteopathic, Dr. Arturo Arroyo* was dark, handsome and athletic, in his early thirties. He was relaxed during the prenatal visit and joked with Stan about golf and playfully teased Carol. It was obvious they had a good rappore. Carol had told me she "intended to stay home until [she] was 10 centimeters"; wanting to "arrive at the hospital pushing". I had suggested that they might consider having a home birth. This way, they could stay home and have the midwife come to them. But this being Stan's first birth and a VBAC for Carol, they said they were not comfortable with that option. I asked Dr. Arroyo if he wanted Carol to come into the hospital sooner rather than later since she was a VBAC. He said "No." He knew I worked as a Midwife's Assistant and I asked if it was okay with him if I monitored fetal hearttones with my fetoscope and checked dilation to assess progress, and he said he had no problem with that. I asked when did he want me to call him. He said, jokingly, "When you are on the way to the hospital...I might be on the golf course and don't want to worry about her and ruin my par." Kidding, I said, "Carol is so determined to stay home until she is complete, I might have to deliver this baby!". We all laughed. I left the office feeling confident they had chosen an excellent doctor and certain that Carol would have her baby the way she invisioned.
The night I was called to Carol's birth, I went to their home and found her working well with the intensity of labor, but her contractions still at irregular intervals lasting less than a minute. Carol was walking and moaning and Stan was doing a beautiful job supporting his wife. Stan's parents were also present, sitting in the kitchen, clearly uncomfortable with Carol not being in the hospital, and genuinely glad to see me. They had waited forty-plus years for the arrival of their first grandchild, and so they anxiously waited a little longer for the time to leave for the hospital. The children were at their dad's house, and Carol's friend Cathy who had flown in from Pheonix, was doing a a great job supporting Carol: keeping her body cool with wet cloths, applying pressure to her back and breathing with her. This was their third birth together and Cathy knew Carol's ryhthm. I listened to fetal hearttones and palpated the baby's position, the baby was ROA. Hearttones were loud and clear and within normal ranges; I timed contractions for a couple hours and found that they were just beggining to get consistently 1 minute long, the point at which we planned to leave for the hospital. I had informed them before the labor of my limited experience doing vaginal- cervical checks, and didn't promise them I would be able to tell accurately what was happening with her cervix, and they were clear I was not a midwife or nurse. Still, they wanted to get some idea of what was going on with her cervix, and wanted to give me the opportunity to learn. In doing an exam, with a sterile glove, I felt the baby's head, deep in the pelvis, at about +1, with smooth, slick texture across the lumpy head of the baby, and no circle of cervix on either side of the head, instead, a half-moon rim of tissue at the top of the head. I was not sure if what I was feeling cervix or not, baffled by the smooth slick feeling across the head ( She said her membranes had ruptured before I arrived), and not finding cervix encircling the head as I had anticipated. I told them I was not really sure what her dilation was but that the baby was pretty low and we should go to the hospital anytime now. Carol said, "I don't want to go yet." I said, "Okay, but we'd better go within the hour." Looking back now, from the vantage point of more experience, I know that what I was feeling was an anterior cervical lip. She was probably 9 centimeters dilated. Cathy and I left Carol and Stan alone. Carol was coping well with the contractions in their jacuzzi bathtub. "She will be a long time yet...last time she went on like this for hours," said Cathy as we sat together on the couch in their livingroom. Ten minutes later, Carol yelled out, "I FEEL AS IF I AM PUSHING!!!" We ran into the bathroom, I helped her onto her feet and walked her to the bed, saying, "let me check you again," and when I did, I found the baby much lower in the pelvis, only an inch from her vaginal opening! "Yep, you are pushing alright, " I said. "There's the baby's head. We've got to go right now!" Carol looked at me and said, "What if I have to push in the car?" I paused before responding to Carol's question for a second that felt like an hour, as I summed up our options. I thought about staying home and catching it myself. No, not a good idea. They did not want a home birth, and besides, if there was a problem, I wouldn't have any emergency equipment, or anyone with more experience to rely upon. I thought about calling the paramedics. I ruled that one out. No reason to create a big emergency, I thought. There is nothing abnormal with her labor going on. I thought about calling a midwife, but she wouldn't have made it on time, the birth was very near. At least if we were on our way, if there was a problem, the hospital would be just minutes away. To many it may seem that we were taking some very big risks, but we were all very confident in Carol and trusting of birth itself, and despite our circumstances, no-one freaked out. As soon as I had considered all the options a feeling of peace washed over me, and I felt assured, clear, calm and certain, which suprised me. I replied to Carol's question, "Well, then I will just have to catch it." And with that, off we went to the hospital, Carol on hands and knees in the back seat of their brand new Chevy Astro-Van, Stan at the wheel, with Cathy and I in the back seat, I at Carol's bottom and Cathy at her head. I asked Stan if he had a cell-phone, wanting to call Dr. Arroyo, and he said, "No. Do you want me to stop at a pay phone?" and I said, "No. Just drive as quickly and safely as you can to the hospital." Carol was moaning, fighting the urge to bear down. I told her to stick her bottom up in the air (to slow the force of gravity which was moving the baby downwards), and blow and pant through the contractions. Her panting gave way to grunting as her body took over the job of pushing the baby. I got out my midwife assistant's birth kit, pulled out my bulb syringe, a deelee suction catheter and a blanket. I was hoping, praying, that I would remember what I had been taught in my neonatal ressuscitation course if I needed to use it. Cathy was so excited. She said "Carol, you are doing it! You are really having your Veebac!!" Just then, I said, "Here comes the head!" Stan, from the driver's seat said, "Great!!!!" I placed my hands on her perineum on each side of the baby's head, and felt it emerge into my hands...I said a prayer to myself "Dear God, please let this baby breathe, Dear God, please let me know what to do if he isn't, Dear God, please don't let these shoulders be stuck, Dear God, let me do what I have been taught to do if they are!" and I reached my hand inside her vagina, right hand against the baby's back at the shoulders, and the baby turned towards my right hand...I heard my midwife-mentor's voice say "I don't worry if my hands reach the shoulders".... I heard myself say, "Okay, give me another push, gently...here comes your baby" (It was odd to hear myself saying the words when it had always been my midwife-mentor saying them), and out slipped the wet warm baby into my arms. I was holding him upside down, "to let the fluids run out" I thought. Then I reached out and felt the cord between my fingers. It was still pulsating. I felt myself relax, saying silently, "Don't freak out. He's getting oxygen still, he doesn't have to breathe on his own and cry right away. We have a minute." (Which felt like an eternity). Just then Cathy noticed that the cord was around his neck, I didn't see this in the dark of the car, while holding the baby face down, blanket covering him. I felt stupid I hadn't noticed that, but grateful Cathy did. It was loose and I slipped over his head easily. I turned him over and then he let out a big wail, and I rejoiced hearing that blessed sound, and was so overwhelmed with gratitude that he was alive and well, I kissed him on the forehead. Just then the van came to a stop, and I noticed we were in the hospital parking lot, outside the emergency room. Stan climbed into the back seat, and I instructed Carol to turn over so she could hold her baby and helping her manuever over the cord which was still attached to the placenta inside of her she did so, and I placed her second son in her arms. Stan, Cathy and I put our arms around each other, enclircling the mother and baby, and we just took a moment, unharried, to look into each others' eyes. We really took in the moment we were experiencing and slowly realized what had just happened. Then I burst out, "You guys, I've never caught a baby before!!!" and they said, "you haven't???" amazedly. The immensity of the moment overwhelmed us. We were laughing and crying and rejoicing that Carol had given birth so easily after two surgical births!  Stan then went to get the ER doctors and nurses who slid open the van door, stepped in with their sterile scissors to cut the cord, and brought a blanket for the baby and wheelchair for the mom. The hospital staff were impressed that the baby was wrapped up and kept warm. "You guys look like you know what you're doing!" they said. "The paramedics don't even bring them in wrapped up!" "Which one of them delivered it?" someone asked. "Her," someone said, pointing to me, "the one with blood on her shirt!"
Stan then went to get the ER doctors and nurses who slid open the van door, stepped in with their sterile scissors to cut the cord, and brought a blanket for the baby and wheelchair for the mom. The hospital staff were impressed that the baby was wrapped up and kept warm. "You guys look like you know what you're doing!" they said. "The paramedics don't even bring them in wrapped up!" "Which one of them delivered it?" someone asked. "Her," someone said, pointing to me, "the one with blood on her shirt!"

The hospital staff were totally amazed to find out she had had two ceseareans and just popped her baby out in the car just like that! Later, the OB nurse scolded Carol for not coming in sooner. Carol and I were shaking and laughing, blown away by what had just transpired. We joked, telling the nurse we needed a strong drink to calm our nerves! The ER doctor delivered the placenta and sewed up her urethral tear. The baby was taken away and evaluated. They quickly brought him back with a clean bill of health. When Dr. Arroyo showed up, I said, "Really, Dr. Arroyo, I was just kidding when I said I'd have to catch the baby!" He said, "That's okay. everything turned out fine. It happens. Mom and baby are alright and that's what matters."
 Baby Joseph had been born on his sister's birthday, just as she had prayed! Carol and Stan made Cathy and I godparents of their son. But what Carol said to me after the birth touched me the most. Having a vaginal birth after a cesearean, she had broken the cycle in her family of birth by cesearean and had "created the possibility for my daughter to birth normally", she said. That was the biggest gift she gave me; allowing me to be part of that momentous transformation!
Baby Joseph had been born on his sister's birthday, just as she had prayed! Carol and Stan made Cathy and I godparents of their son. But what Carol said to me after the birth touched me the most. Having a vaginal birth after a cesearean, she had broken the cycle in her family of birth by cesearean and had "created the possibility for my daughter to birth normally", she said. That was the biggest gift she gave me; allowing me to be part of that momentous transformation!
Carol couldn't feel 100% comfortable giving birth in the hospital, but she wasn't prepared to have a homebirth either. While she didn't plan it this way, she ended up with the middle ground--in her car, halfway between home and hospital! They are planning to get pregnant again and they said they wouldn't do it without me. They are considering a homebirth with a midwife in attendance so they and just stay in bed and have their baby! They ordered license plates for their new van which read:

* Name has been changed.
"My supervising midwife was always by my side, calm and clear and reassuring, reminding me of what to watch for.. her constant guidance through every step and her confidence in my abilities gave me such an empowered feeling of pride and belief in myself."
I am an apprentice midwife, and have worked assisting midwives at homebirths for several years and have been honing my skills doing hospital labor support, taking workshops, studying my academics and and learning as much as I can on-the-job from the masterful midwives I assist.
Ingrid and Boris called me late in her pregnancy looking for a labor companion to help them give birth in a hospital. I liked them both immensly when we met for an initial interview and we talked for a couple hours about all sorts of topics--unrelated to birth. I liked them, and they liked me. It was a good match. I agreed to be their labor companion. She is Swedish and had had her first child five years earlier without any drugs or episiotomy in a Swedish hospital with midwives and a birthing pool available. Our birth centers in the U.S. are much more like the environment in which she gave birth in her country, and Ingrid was suprised to find out how conservative American hospitals are by comparison. She would have preferred a birth center or homebirth for this birth, but she had so much trust in her body and the birthing process itself that she didn't think that a hospital birth was going to be an issue until she had started asking questions of her doctors. As she formulated her birthing plan, she was to get a rude awakening about the differences between the American and Scandanavian maternity systems. Ingrid wanted to walk in labor, drink juice, be free of an IV, to have her five year old son present at the birth, to have her baby placed on her tummy--and found that her doctors were very intractible and unsupportive of her desires. She considered switching to a more progressive hospital and doctor or a birthing center, but since she had an H.M.O., she couldn't switch so late in the pregnancy. Furthermore, her husband was becoming more and more uncomfortable with the idea of having to try and "negotiate" with doctors who were so obduriate; whose liability issues dominated their practices.
Two weeks prior to their due date, when we went into the doctor's office and they asked for final approval of their birth plan, the doctors told her that she had to be in the bed on the electronic fetal monitor continiously once her cervix reached 5 centimeters of dilation and that her son could not be at the birth, even with supervision. Ingrid was clearly upset about the restrictions they were making on her and felt that she would not be comfortable laboring on her back in bed, as she had walked throughout her labor last time. I negotiated a plan with the doctor to allow Ingrid to be on the monitor continiously (her doctor's condition) but standing next to or leaning into the bed (the only way she could tolerate hard contractions). Her doctor agreed to this only if the head of the baby was deep into her pelvis; or fear of cord prolapse with a high head. I assured the couple that I would do my best to help them stay at home until active labor was established (contractions 3 minutes apart, lasting 45 seconds for at least one hour), and as I live only five minutes from them, and the hospital is equally as close, this was a feasible plan. I told them I would try and assess their dilation and would listen to the baby's heartbeat with my doppler while we were at home. (They knew that I am not a fully-trained midwife or nurse, but rather an Apprentice Midwife and that I am still learning to do cervical checks). They seemed to appreciate my honesty about my level of experience, though, and wanted to have another way of telling how Ingrid was progressing other than the contractions. We were all very distressed by the hostility and intractibilty of the doctors; and I felt that my capacity to negotiate on their behalf was going to be limited, as the doctors were not intrested in working cooperatively with them or me. We got the feeling the doctors would have preferred that they were not their patients. It was not an ideal situation, but I assured them we'd make the best of it if the hospital was where they chose to give birth. We also discussed the pros and cons of having a homebirth--that was where Ingrid beleived she'd be the most comfortable, and Boris realized the truth of my words when I said " A woman gives birth the easiest where she feels most comfortable and with people she trusts".
So, that is how, two week prior to their due date, they decided to have the baby at home, and to give me the opportunity for my first supervised delivery. Their doctors actually pushed them into having the birth they wanted. I called my senior midwife, who is licensed by the state and has fifteen years experience. I asked her if she would supervise my doing the birth. After meeting with the couple, reviewing their records from the previous birth and finding no risk factors for homebirth based on her current prenatal records and condition, seeing the trust in birth the couple had and their comfort with childbirth at home, my mentor agreed to be accountable for the birth.
With the new birth team was in place, Ingrid felt safe she could let go and have her baby. She did so beautifully. At home, laboring throughout the night while her son and ninety-one year old father-in-law slept, all was peaceful and quiet. I did all the assesments of her progress and the baby's well-being with my mentor's supervision. She sat by my side, calmly asking the pertinent questions, such as "Is there cervix on the left?", "Do you feel any bag?" "How high is the baby?". I asked her if she wanted to check after me to be sure I was accurate, but she responded with "no, I believe you." She told me later that she can do that because she trusts I will tell her if I don't know something. It was so empowering for me to know that I knew the answers and had skills sufficient to make correct assessments. We had the emergency equipment all set up and ready to be used in case anything unexpected came up, and the hospital was only five minutes away, but we knew nothing wouldn't need to use it, as this Birthing Goddess was so trusting of birth and we had complete faith in her ability to give birth normally; we knew she would not manifest any complications.
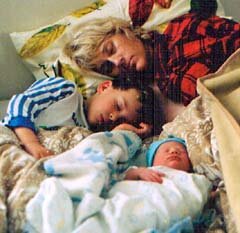
I was thrilled to feel the dilation and effacement of her cervix and stretching of her bag of waters, the baby's fontanelles, to know the baby's position and to feel her body connecting to my instructions on how to bear down as she effectively pushed her baby out into my eager hands, supported by her husband from behind.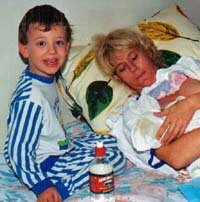 My supervising midwife was always by my side, calm, clear and reassuring. Her confidence and belief in my abilities was truly empowering. She asked me all the important questions; and giving me all the reminders I needed in order to be watchful: "Is there a cord?", "Is she bleeding?". Boris and Ingrid's second son, Sven, was born in the wee hours of the morning of the New Year, with a big wail and rosy color. They woke up their older son, Lars, saying, "your brother's here!" and then basked in wonderment of the new addition to their family.
My supervising midwife was always by my side, calm, clear and reassuring. Her confidence and belief in my abilities was truly empowering. She asked me all the important questions; and giving me all the reminders I needed in order to be watchful: "Is there a cord?", "Is she bleeding?". Boris and Ingrid's second son, Sven, was born in the wee hours of the morning of the New Year, with a big wail and rosy color. They woke up their older son, Lars, saying, "your brother's here!" and then basked in wonderment of the new addition to their family.
As the family got acquainted with each other, my mentor and I checked her perineum for tears. Although I had given counterpressure as the baby's head emerged, the baby's hand had been born along side a pretty large head. We discovered that Ingrid had a moderate tear. My mentor demonstrated the suturing technique ( I had sutured in a classroom setting, but never on an actual woman), and then let me do the repair, with her constant guidance through every step; her confidence that I could do it accurately gave me a feeling of pride and belief in myself.
 After the birth, the parents were gushing with appreciation, remarking how ideal it was to give birth in the privacy of their home, to be left alone to labor as they pleased--sitting in a chair, soaking in the bathtub, sipping juice, walking. I expressed my appreciation for the opportunity they gave me, letting them know that I would be grateful to them forever. I told my mentor I could not thank her enough for the opportunity and for her confidence in me. I let her know what a wonderful teacher she is, because she didn't have to take control, she could allow me to learn (of course, she could have taken over if there had been an emergency). She assured me that I did a really, really good job and that all I need is more hands-on experience to progress towards my goal.
After the birth, the parents were gushing with appreciation, remarking how ideal it was to give birth in the privacy of their home, to be left alone to labor as they pleased--sitting in a chair, soaking in the bathtub, sipping juice, walking. I expressed my appreciation for the opportunity they gave me, letting them know that I would be grateful to them forever. I told my mentor I could not thank her enough for the opportunity and for her confidence in me. I let her know what a wonderful teacher she is, because she didn't have to take control, she could allow me to learn (of course, she could have taken over if there had been an emergency). She assured me that I did a really, really good job and that all I need is more hands-on experience to progress towards my goal.
The apprenticeship model of training midwives in an ancient tradition and there is nothing better than that one-on-one mentoring. It is with this care and guidance that great midwives are developed. My teacher is a product of that mentoring herself, and that is why she knows it is an ideal way to learn a trade. I hope that all aspiring midwives will have the opportunity to find their perfect teachers-birthing mothers and wise woman mentors alike-as I have.

Love,
Baby Sven"
I was doing my first primary prenatal care with a past client - now friend (This was her 6th pregancy, babies #7 and #8). This pregnancy was a surprise and seemed like the perfect "first" for me as she was a repeat client and a very responsible couple - easy birther. WELLLLL.... at about 34 weeks we were certain that she was either a month off on dates or we needed to talk seriously about the possibility of twins. Sure enough at the next prenatal we detected two very different heart beats - the couple laughed and shared with us that they had dual hick-ups going the night before.
Story continued by clicking here: birthtales2.htm